- Part 1: 2022 Star Ratings Release
- Part 2: The Importance of CAHPS
- Part 3: Decision Point CAHPS Compare Dashboard
- Part 4: Decision Point CAHPS Improvement Solution
2022 Star Ratings Release
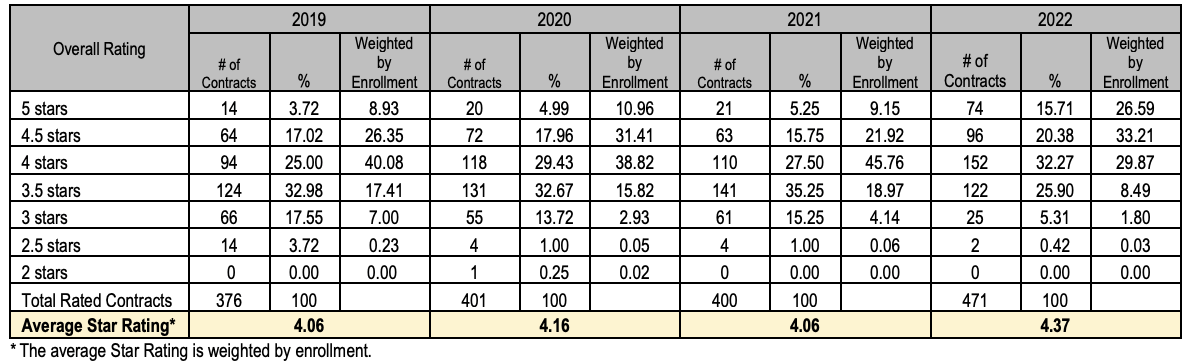
Last week, CMS released its 2022 Star Ratings designed to measure the experiences Medicare beneficiaries have with their health plan and health care system. Health plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
This year saw the greatest number of 4, 4.5, and 5 Star achieving plans on record, undoubtedly helped by the Interim Final Rule.
In light of the pandemic, CMS said it “wanted plans to have some degree of certainty related to Star Ratings program requirements,” and it wanted to make sure plans were focused on providing care for beneficiaries. The agency traditionally calculates Star ratings based on measure data from the prior year, though it used 2020 data in calculating 2022’s scores to account for pandemic disruptions. By Star measure year 2023, we expect to see CMS make efforts to correct course, making the Stars program as competitive as ever.
The Importance of CAHPS
One of the integral assessment categories within the Star Rating system is a Consumer Assessment of Healthcare Providers & Systems (CAHPS) survey. CMS requires all MA and PDP contracts with at least 600 enrollees to have their members surveyed by an approved vendor to measure their members’ experience and satisfaction with the plan based on the quality of care they’ve received in the past 6 months.
With the Interim Final Rule in play, making it impossible for plans to receive a rating lower than their 2021 rating, we saw many plans sustain their overall CAHPS ratings and many plans opting to use the more recent CAHPS data in order to elevate their scores. There was a slight uptick across the national averages of all CAHPS measures with the exception of Getting Needed Care that dropped from an 83.13 for 2021 to an 83.01, likely due to pandemic related factors.
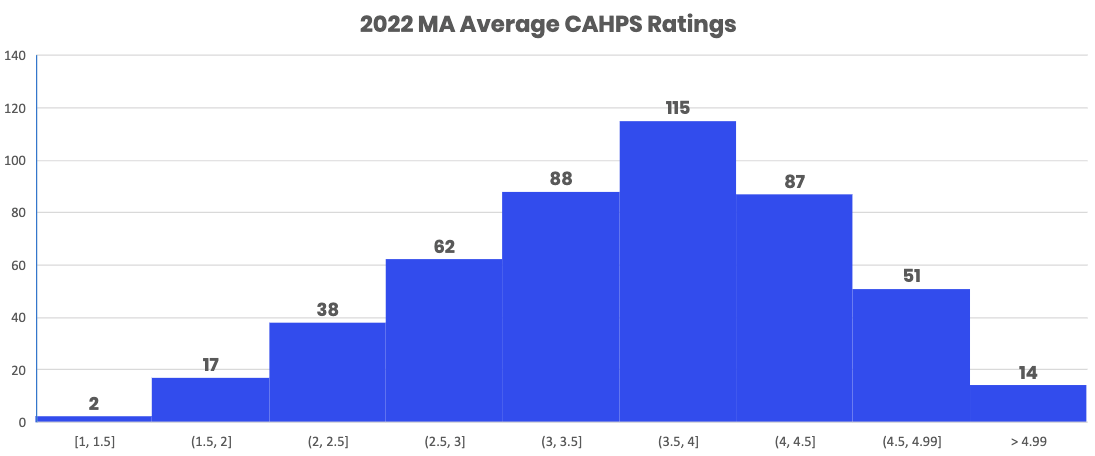
As many of us are aware, CMS is increasing the weighting of the CAHPS measures for its Medicare Star program. By Stars 2023 (plan year 2022), the CAHPS measure grouping will double in weight and become the single most important measure grouping for all of Medicare Star - CAHPS will account for 32% of Stars (contrasted with HEDIS which will account for 15% of Star and HOS which will account for 9% of Star). In fact, if CAHPS is grouped with all the Star member experience measures (such as members choosing to leave the plan and others), member experience as a measure group will account for 54% of Star. It is safe to say that plans that fail at member experience do not have a path of achieving or maintaining 4+ Stars, which may result in a lack of market competitiveness.
Decision Point CAHPS Compare Dashboard
To help you understand how you rank within your service areas, our CAHPS team developed a 2022 CAHPS Compare Dashboard that you can use to analyze this year’s CAHPS results and compare your performance to competitors in the states and counties that you operate in.
For instance, our team recently leveraged the dashboard to compare one of our clients, SelectHealth, to other plans within their primary market.
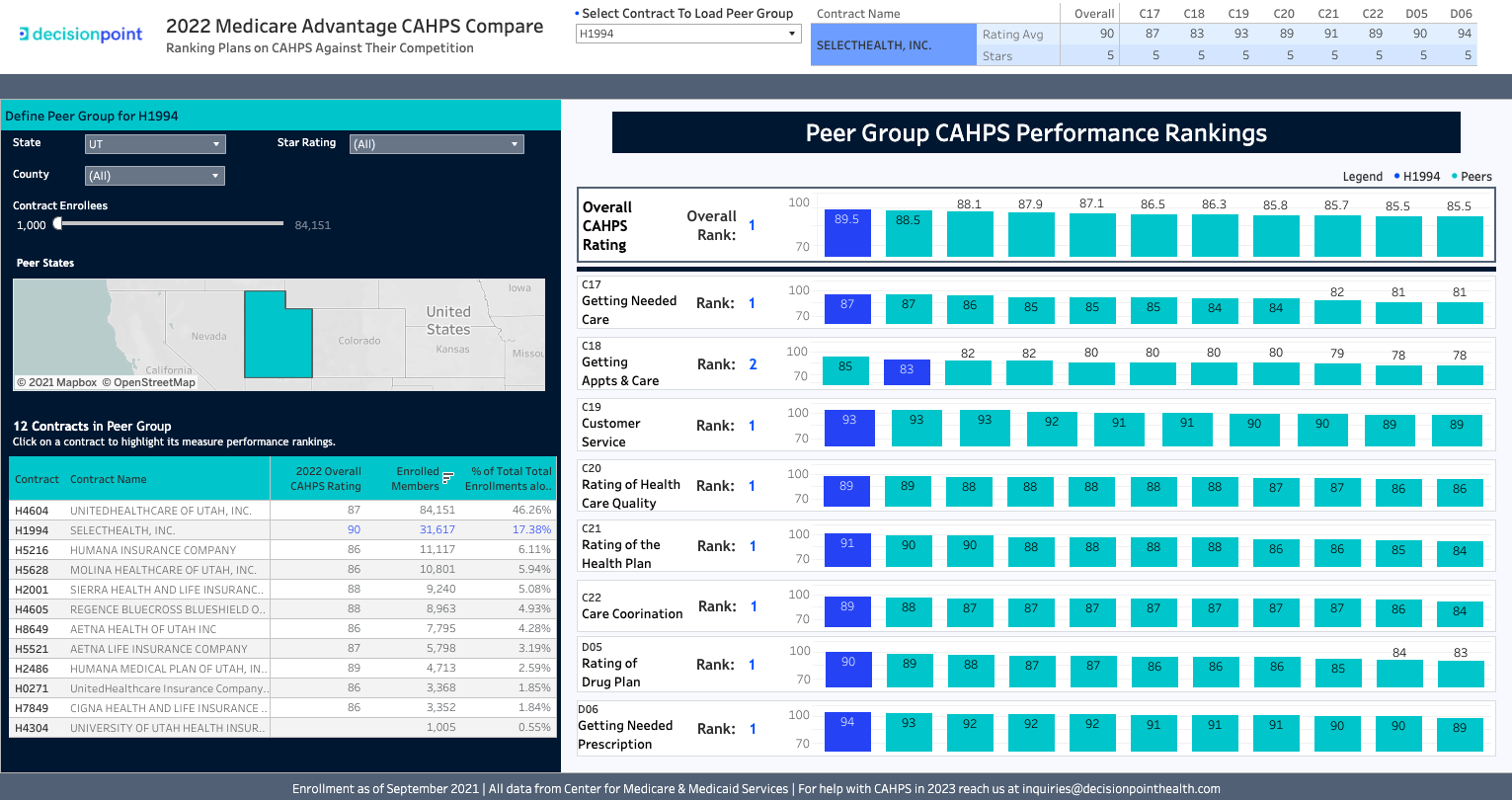
You can access it here – please feel free to share it with your team!
At Decision Point, we understand that given the anonymized nature of the CMS survey process, CAHPS measures are among the most challenging measures to improve. We do not know who was targeted for the CAHPS survey last year, who responded, or how they responded.
This is not the case for CAHPS. Given the importance of achieving Star success, it is critical for healthcare organizations to be able to understand CAHPS at a member level. To make a real impact, we need to discover which members will rate their experience poorly and take appropriate action.
Decision Point CAHPS Improvement Solution
Decision Point has 5-step process that has helped our clients improve CAHPS and achieve 5-Stars:
- Behavioral Prediction: Predict CAHPS and member experience for every member and every measure
- Optimization: Identifies the ideal members for engagement that will yield maximum CAHPS and member experience impact
- Segmentation: Population segmentation using a range of characteristics and risk predictions
- Engagement: Everything a plan needs to take action, including optimized CAHPS scripts for each outreach channel that are based on deep behavioral science research and campaign intelligence
- Impact Measurement & Reporting: Understand the drivers of CAHPS and member experience and measure the impact of outreach to outcomes
To learn about how we help our clients take control of their CAHPS scores and to discover how many members per contract you’ll need to engage with in order to meet your CAHPS goals to maintain competitiveness in the markets you serve, you can click here to set up some time with one of our CAHPS experts.