- Part 1: 2023 Star Ratings Release
- Part 2: Decision Point CAHPS Compare Dashboard
- Part 3: Decision Point CAHPS Improvement Solution
2023 Star Ratings Release
Last week, CMS released its 2023 Star Ratings designed to measure the experiences Medicare beneficiaries have with their health plan and health care system. Health plans are rated on a scale of 1 to 5 stars, with 5 being the highest.
This year’s Star ratings release shows that record increases in plans with high Star ratings are on the decline as several pandemic related regulatory flexibilities are going away in 2023. The importance of the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey and associated member experience measures shines through as their quadruple weights are realized.
💡 With the absence of the CMS pandemic provisions for 2023 Star, the number of 5-Star contracts fell significantly from 74 in 2022 to 57 for the coming year.
The impending removal of a disaster provision put in place to help plans in response to the COVID-19 pandemic has brought us back to Star reality. The provision gave plans the opportunity to opt for the “better of” on 28 quality and performance measures, allowing them to choose the best score, giving many plans a welcomed boost to their performance. The result was 2022 being the year that produced the greatest number of 4, 4.5, and 5-Star achieving plans on record.
The added weight on the CAHPS survey has given a sizeable advantage to plans that excel on CAHPS.
💡 Of the 57 5-Star overall plans for 2023, 51 had an average CAHPS rating of 4.5 or higher.
💡 Of the 193 plans that averaged a rating of 4 or higher across CAHPS measures - all but 16 achieved a 4 Star overall rating and will receive their QBP.
💡 4/5 plans that improved their overall Star rating did so by improving on CAHPS.
💡 92% of plans that improved overall Star for 2023 maintained or improved their CAHPS scores YoY.
Additionally, CMS introduced guardrails for all measures that have been in the rating program for more than three years, except for the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey and improvement measures.
“Guardrails are bi-directional caps that restrict upward and downward movement of a measure’s cut points for the current year’s measure-level Star Ratings compared to the prior year’s measure-threshold specific cut points,” CMS wrote.
Despite the reductions, the overall outlook is a positive one as the number of 5, 4.5, and 4-star Medicare Advantage plan contracts is higher for 2023 than just two years ago, in 2021.
Decision Point CAHPS Compare Dashboard
To help you understand how you rank within your service areas, our CAHPS team developed a 2023 CAHPS Compare Dashboard that you can use to analyze this year’s CAHPS results and compare your performance to competitors in the states and counties you operate in.
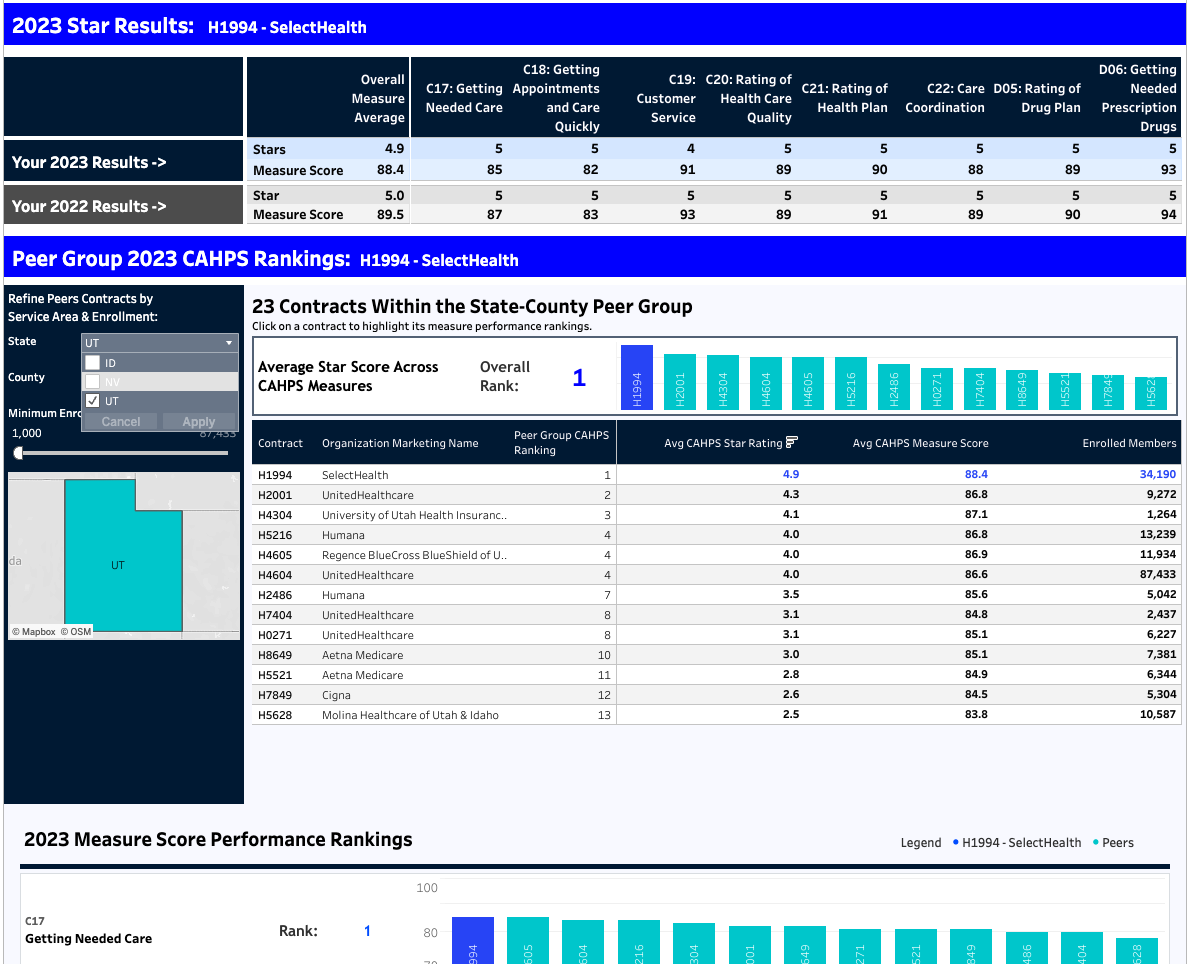
You can access it here – please feel free to share it with your team!
At Decision Point, we understand that given the anonymized nature of the CMS survey process, CAHPS measures are among the most challenging measures to improve. We do not know who was targeted for the CAHPS survey last year, who responded, or how they responded.
This is not the case for CAHPS. Given the importance of achieving Star success, it is critical for healthcare organizations to be able to understand CAHPS at a member level. To make a real impact, we need to discover which members will rate their experience poorly and take appropriate action.
Decision Point CAHPS Improvement Solution
Decision Point has a 5-step process that has helped our clients improve CAHPS and achieve 5-Stars:
- Behavioral Prediction: Predict CAHPS and member experience for every member and every measure
- Optimization: Identifies the ideal members for engagement that will yield maximum CAHPS and member experience impact
- Segmentation: Population segmentation using a range of characteristics and risk predictions
- Engagement: Everything a plan needs to take action, including optimized CAHPS scripts for each outreach channel that are based on deep behavioral science research and campaign intelligence
- Impact Measurement & Reporting: Understand the drivers of CAHPS and member experience and measure the impact of outreach to outcomes
